Bringing a baby into the world is powerful, emotional, and life-changing, but it also takes a real toll on the body and mind. After delivery, most attention naturally shifts to the newborn, while the mother quietly begins one of the most important phases of her journey: healing. This is where postpartum recovery tips truly matter. Recovery is not about rushing back to normal; it’s about allowing your body the time, care, and support it needs to heal in a healthy way.
Every mother’s recovery looks different. Some feel physically stronger within weeks, while others take months to feel balanced again. Both are completely normal. This guide is written to gently support new parents and caregivers with practical, realistic, and compassionate advice to help healing feel less confusing and more manageable.
What Postpartum Recovery Really Means
Postpartum recovery refers to the physical, emotional, and hormonal changes a woman experiences after childbirth. This period often lasts six weeks medically, but real recovery can take much longer. During this time, the uterus shrinks back to its original size, hormone levels drop rapidly, muscles stretch and repair, and emotions fluctuate.
Medical resources such as MedlinePlus explain that postpartum care includes monitoring physical healing, emotional well-being, and overall adjustment to motherhood, not just the first few weeks after birth:
Understanding that recovery is layered helps reduce guilt and unrealistic expectations. You’re not “behind” if you’re still sore, tired, or emotional weeks after delivery, you’re healing.
Postpartum Recovery Tips Every New Mom Should Know
When it comes to healing, small daily habits matter more than big changes. These postpartum recovery tips focus on protecting your energy, supporting your body, and creating space for emotional adjustment.
- Rest whenever possible, even in short breaks
- Eat nourishing meals consistently
- Ask for help without guilt
- Listen to your body’s signals
- Avoid comparing your recovery to others
Healing faster doesn’t mean doing more, it means doing what truly supports recovery.
Rest Is the Foundation of Healing
Sleep deprivation is one of the biggest challenges after childbirth. While uninterrupted sleep may not be realistic, rest still plays a critical role in healing tissues, stabilizing mood, and restoring strength.
Think of rest as recovery time, not inactivity. Sitting instead of standing, lying down while feeding your baby, or simply closing your eyes for ten minutes can make a difference. Overexertion in the early weeks can slow postpartum recovery after birth and increase discomfort.
Health organizations like the World Health Organization emphasize that maternal rest after childbirth is essential for preventing complications and supporting long-term well-being.
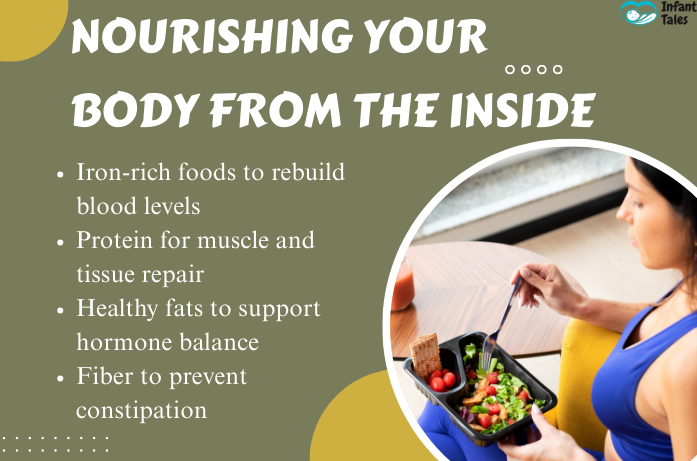
Nourishing Your Body From the Inside
Food is one of the most powerful tools for healing. Your body has lost blood, used energy reserves, and undergone physical stress. Replenishing nutrients helps speed tissue repair and stabilize energy levels.
Focus on:
- Iron-rich foods to rebuild blood levels: spinach, lentils, beetroot, dates, jaggery, eggs, lean meats
- Protein for muscle and tissue repair: dal, chickpeas, beans, paneer, tofu, yogurt, eggs, fish, chicken
- Healthy fats to support hormone balance: nuts, seeds, homemade ghee, olive oil, avocados, fatty fish
- Fiber to prevent constipation: oats, whole grains, fruits, vegetables, flaxseeds, chia seeds
These choices act as natural postpartum healing tips, supporting recovery without pressure. Hydration is equally important, especially if you are breastfeeding, as dehydration can increase fatigue and slow healing.
The mayo clinic highlights the importance of balanced nutrition during the postpartum period for maternal recovery.
Gentle Movement Supports Circulation
Complete inactivity is not always helpful. Gentle movement, when approved by a healthcare provider, improves circulation and reduces stiffness.
Short walks around the house, slow stretching, and simple breathing exercises are often safe in the early weeks. These movements help prevent blood clots and support overall comfort without straining the body.
Avoid heavy exercise, abdominal strain, or lifting until your doctor confirms it’s safe. Healing is not about pushing through pain, it’s about respecting limits while learning how to recover after childbirth safely.

Caring for the Body After Delivery
Physical recovery looks different depending on how you gave birth. Paying attention to wound care and hygiene helps prevent infection and speeds healing.
For vaginal births, soreness and swelling are common. Keeping the area clean, using warm water, and resting frequently can ease discomfort. For C-sections, incision care and avoiding strain are essential. Any increase in pain, redness, or discharge should be discussed with a healthcare provider.
Proper postpartum care for new moms includes understanding that discomfort is normal, but worsening pain is not. Resources from the National Institutes of Health explain that proper wound care, hygiene, and activity limits reduce infection risk and promote healing:
Hormonal Changes and Emotional Healing
One of the most surprising parts of postpartum recovery is how emotional it can feel. Hormone levels drop sharply after delivery, which can lead to mood swings, tearfulness, or anxiety.
Many mothers experience “baby blues” in the first two weeks. These feelings usually resolve on their own with rest and support. However, if sadness, fear, or emotional numbness lasts longer or interferes with daily life, it may signal a postpartum mood disorder.
The CDC explains that postpartum depression and anxiety are medical conditions, not personal failures. Emotional healing deserves the same care as physical recovery.
Understanding Postpartum Body Changes
The body does not immediately return to its pre-pregnancy state, and that is normal. Weight changes, stretch marks, abdominal softness, and joint looseness are part of postpartum body recovery.
Your organs are shifting back into place, muscles are repairing, and connective tissues are adjusting. This process takes time. Expecting immediate physical changes can increase stress and slow emotional healing.
Be patient with your body. It has done something extraordinary. American Pregnancy Association resources emphasize that postpartum recovery is gradual and varies widely among women:
Pelvic Floor and Core Awareness
Pregnancy and childbirth stretch the pelvic floor muscles, which support the bladder, uterus, and bowel. Weakness can cause leaking urine, discomfort, or pressure sensations.
Gentle pelvic floor exercises, when approved by a doctor, can support recovery. Avoid straining, especially during bowel movements, and do not rush into intense workouts.
In some cases, working with a trained professional can help rebuild strength safely. Protecting this area is a key part of long-term recovery.
The Role of Self-Care in Healing
Self-care doesn’t have to be elaborate to be effective. Simple habits like showering, stepping outside for fresh air, or taking a quiet moment can restore a sense of control and calm. Caring for yourself after delivery.
Practical postpartum self care tips include:
- Keeping expectations realistic
- Limiting visitors if needed
- Eating regularly
- Speaking kindly to yourself
Self-care is not selfish, it supports healing and emotional balance.
When to Seek Medical Help
While discomfort and fatigue are normal, some symptoms require immediate medical attention. Contact a healthcare provider if you experience:
- Heavy bleeding that soaks a pad in an hour
- Fever or chills
- Severe or worsening pain
- Foul-smelling discharge
- Persistent sadness or intrusive thoughts
Early care can prevent serious complications and protect long-term health.
Frequently Asked Questions
1. How long does postpartum recovery take?
Initial physical healing often takes about six weeks, but full recovery, especially emotional and hormonal balance, can take several months. Every mother’s body heals at its own pace.
2. Is it normal to feel overwhelmed after delivery?
Yes, feeling overwhelmed is very common. Hormonal shifts, lack of sleep, physical healing, and adjusting to a new routine can all affect emotions during the postpartum period.
3. Can I speed up recovery naturally?
You can support healing by resting as much as possible, eating nourishing foods, staying hydrated, doing gentle movement when approved, and accepting help from others.
4. When should I contact a doctor during postpartum recovery?
You should seek medical advice if you experience heavy bleeding, fever, severe pain, signs of infection, or ongoing sadness or anxiety that does not improve after a couple of weeks.
5. Is it normal for my body to feel different months after childbirth?
Yes, it is normal. Changes in weight, muscle tone, energy levels, and emotions can continue for months as your body gradually adjusts after pregnancy and delivery.
Final Word
Recovery after childbirth is not something to complete or rush through it is a gradual, deeply personal process that unfolds in stages. Some days you may feel stronger and more confident, while other days your body or emotions may ask you to slow down. This back-and-forth is a normal part of healing, not a setback. True recovery happens when rest, nourishment, patience, and support come together over time.
At Infant Tales, we believe that caring for a baby begins with caring for the parent. Honoring postpartum recovery means recognizing that healing includes physical strength, emotional balance, and mental well-being. There is no perfect timeline and no “right” way to recover only what feels right for your body and your life.
Give yourself permission to heal at your own pace. Ask for help when you need it, celebrate small improvements, and trust that your body knows how to recover. You are adjusting to a new chapter while healing from an incredible experience. That takes strength, grace, and time and you are doing better than you realize.
Medical Disclaimer: This article is for informational purposes only and does not replace professional medical advice. Always consult a qualified healthcare provider for concerns related to postpartum recovery or maternal health.



